Gender-Affirming Surgeons’ Attitudes toward Social Media Communication with Patients
Jules L. Madzia , Tee Chuanromanee , Gaines Blasdel , Aloe DeGuia , Mary Byrnes , Nabeel A. Shakir , Megan Lane , Oliver L. Haimson
Online spaces are increasingly important for transgender people who are considering gender-affirming surgeries to find information, ask questions, and communicate with each other. While many surgical resources are community-generated, the onus of providing medical information about surgery should be on the surgical team. We sought to understand the potential for an online space for surgeon and community engagement. We assessed gender-affirming surgeon perspectives on online communication and communities by conducting a survey (N = 55) to understand current social media use and gauge surgeons’ opinions related to participating in online spaces. We found that gender-affirming surgeons were not generally in support of a new online platform for patient-surgeon communication, with 67% responding that a new platform was not needed. Participants identified potential negative implications including risks to patients (e.g., misinformation, liability, and platform use in emergency situations) and risks to surgeons (e.g., the additional burden that the platform would place on their already-limited time, changes to surgeon culture, and safety concerns related to online harassment). Potential positive implications include opportunities to improve patient education and enhance patient care. Our results establish empirical understanding of social media use patterns among gender-affirming surgeons and may inform the design of resources to enable trans patients to receive the information and care that they require when considering and undergoing gender-affirming surgery.
- Volume (Issue)
- 2(3-4)
- Published
- December 15, 2023
- DOI
- 10.57814/e1tc-mt51
- Copyright
- © 2023. The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0)
- Preferred Citation
- Madzia, Jules L., Chuanromanee, Tee, Blasdel, Gaines, Aloe, DeGuia, Byrnes, Mary, Shakir, Nabeel A., Lane, Megan, Haimson, Oliver L.. 2023. "Gender-Affirming Surgeons’ Attitudes toward Social Media Communication with Patients ." Bulletin of Applied Transgender Studies 2 (3-4): 151-174. https://doi.org/10.57814/e1tc-mt51
Online spaces such as social media sites are increasingly important for transgender people who are considering gender-affirming surgeries to find information, ask questions, and communicate with each other (Augustaitis et al. 2021; Chuanromanee and Metoyer 2021). For instance, many trans people gather to discuss surgeries in communities on sites like Reddit, Discord, Facebook, and on trans-specific sites like TransBucket and ModClub. These spaces fill critical knowledge gaps that have been identified including information on long-term outcomes, clinic safety, and preoperative requirements. Online spaces are vital for community-building and filling needs unmet by the medical establishment.
While many surgical resources are community-generated, the onus of providing medical information about surgery should be on the surgical team. Yet in an increasingly hostile political environment for both trans patients and gender-affirming care providers, those who disclose personal information about gender affirming surgery online may have greater risk for experiencing harassment, mistreatment, or misappropriation of their information. Patients and surgeons need safe online spaces where they can communicate without fear of harassment and abuse. Additionally, in patient-only online spaces, there is potential for misinformation about gender-affirming surgeries to circulate, usually from well-meaning but ill-informed community members and allies (Augustaitis et al. 2021). Many trans people considering surgery would value the opportunity to communicate online with gender-affirming surgeons, who can provide factual information and lend expertise to combat faulty claims that may arise in these spaces (Augustaitis et al. 2021; Chuanromanee and Metoyer 2021).
As a further barrier to care, there is a paucity of gender-affirming surgeons, and many patients travel long distances (even internationally) and spend months or years on waiting lists for surgery. Those who do have local surgical teams typically do not have more than one choice, outside of the few largest cities in the United States and may lack access to specific techniques. While there was a relative increase in access to non-local providers during COVID-19 due to changes in telehealth rules (U.S. Dept. of Health and Human Services 2023), many providers have returned to requiring in-person consultations, costing additional financial and time resources. Increased access to formal, freely available information from gender-affirming surgical teams can help inform patient decision making in a cost-effective and efficient manner.
We sought to understand the potential for an online space for surgeon and community engagement. As a first step, we assessed gender-affirming surgeon perspectives on online communication and communities. We conducted a survey (N = 55) to gauge surgeons’ opinions and concerns related to participating in such a space. We found gender-affirming surgeons were generally not in support of a new online platform for patient-surgeon communication, with 67% responding that a new platform was not needed. Private practice surgeons and those who currently frequently used social media were more likely to support such a platform. Participants also provided potential negative and positive implications of a new platform facilitating patient-surgeon communication. Potential negative implications include risks to patients, such as misinformation, liability, and platform use in emergency situations, and risks to surgeons, such as the additional burden that the platform would place on their already-limited time, changes to surgeon culture, and safety concerns related to online harassment. Potential positive implications include opportunities to improve patient education and enhance patient care.
This work contributes an empirical understanding of gender-affirming surgeons’ social media use and their attitudes toward using an online platform designed to facilitate communication with trans patients considering surgery. Our results will inform the design of future resources to enable trans patients to receive the information and care that they require when considering, researching, undergoing, and recovering from surgery.
Health Information Sharing in Online Trans Communities
Online health communities are important sources of health care information for patients, empowering them to make informed choices about their health (Nath et al. 2016). Benefits of online health communities include psychosocial support for patients and their caregivers as well as information support from peer patients and online community moderators (Gustafson et al. 2001; Huh et al. 2013). Social media is a valuable tool for the transgender community in particular for finding resources and information, decision-making, and making connections with others (Augustaitis et al. 2021; Chuanromanee and Metoyer 2021). These platforms allow people to share their experiences (Darwin 2017; Yeadon-Lee 2016) and exchange information, and most online groups provide a level of anonymity and safety to their members (Haimson et al. 2020).
Patients’ and physicians’ perspectives in online communities are quite different, and communication with peers addresses different needs (Hartzler and Pratt 2011; Huh 2015). Despite the benefits of online information-sharing, it can be difficult for patients to find validated, non-conflicting information given the volume of information that exists online (Eysenbach 2003). Increased involvement from physicians in online health communities could help address some of these limitations (Kim and Mrotek 2016; Kim and Shyam Sundar 2014). Limited prior research has examined the potential for physician involvement in online health communities to help address some of these issues, and found that clinical expertise is sorely needed in online health communities to help with clarifying medical information and helping patients understand what to expect with regard to particular health conditions and procedures (Huh and Pratt 2014). Physician engagement in online knowledge-sharing may be increased if there are practical benefits to their contributions such as enhanced reputation, greater likelihood that patients will seek future consultations, and monetary rewards (Zhang et al. 2022). Evidence demonstrates that platforms that have physicians who actively engage in information-sharing attract more patients, incentivizing online platforms to foster collaborations with physicians (Ma et al. 2022).
Physician Participation in Health Information Sharing
Physicians have both Health Insurance Portability and Accountability Act (HIPAA)-compliant and non-compliant means of communication with patients. Over the past decade, physicians have increasingly utilized HIPAA-compliant patient portals integrated with electronic health records to communicate with patients. This form of interaction has grown significantly following the COVID-19 pandemic, with recent single-center experiences reporting 71% of patients interacting with their hospital center utilize a patient portal (Lo et al. 2022). These messages primarily discuss medical needs, with an estimated 68% containing decision making tasks (Robinson et al. 2017). While patient portals have become a key tool for improving accessibility and continuity of care, some speculate increases in patient communication via patient portals are tied to physician burnout (Mehrotra et al. 2020; Zarefsky 2023).
Beyond formal systems integrated with the electronic medical record, some physicians interact with patients via advertising or communicating directly on social media. While surgeons have a demonstrated academic interest in social media use in general, this has not translated to gender-affirming surgery (K.G. Bennett et al. 2018). Among plastic surgery programs, gender-affirming care takes up a very small portion—less than 2%—of social media posts (Maisner et al. 2023). Analysis of gender-affirming surgery content on YouTube and Tiktok suggest over two thirds of content concern patient experience (Song et al. 2022). Despite the low production of content, gender-affirming providers use social media to engage with trans communities (such as by following trans accounts, answering questions, and helping to spread accurate medical information) to better understand trans lived experiences, which can help them to provide better care (Blotner and Rajunov 2018). However, the rate of social media use for these purposes, and granular information about social media use amongst gender-affirming surgeons, is unknown. Some physicians are consumers of social media, but there is a paucity of surgeon-produced content in gender-affirming surgery.
Beyond patient portals and social media, novel digital tools such as mobile health applications regarding surgery have typically been developed as an extension of an established individual patient-physician relationship, and the majority of platforms identified in a 2019 systematic review focused on post-operative communication or structured reporting of symptoms (De La Cruz Monroy and Mosahebi 2019). One tool was identified as including preoperative communication, and use of this tool was later found to correlate with fewer surgical cancellations (Stewart et al. 2019). Other than mobile health applications, Wellprept has been described as a digital tool for surgeons to provide standard pre-operative information to patients in advance of consultation appointments, such that more of the appointment can be utilized discussing patient-specific concerns (Stork 2023). In gender-affirming surgery specifically, there is novel development of online decision aids in masculinizing genital surgery to assist with surgical consultation (Scalia et al. 2021).
Methods
Recruitment
Physicians who perform gender-affirming surgery in the United States or Canada with an available email were eligible for this study. We created a list of gender-affirming surgeons by gathering names from two publicly available sources: the member directory for the World Professional Association for Transgender Health, and transhealth.org. Contact information was obtained through online sources such as practice websites, academic articles, and (in cases where contact information was not publicly available) personal contacts of the authors. The project was deemed exempt from ongoing review by the University of Michigan Institutional Review Board (IRBMED HUM00218192).
Survey
To understand physician perceptions of social media and possible use of a new platform, participants completed an electronic survey with both ad-hoc elements and subscales of an instrument examining social media use developed by McGowan et al. (2012; Supplemental 1). This Likert-based instrument is informed by the Technology Acceptance Model and was validated in primary care physicians and oncologists. We utilized multiple subscales in this instrument including frequency of social media use, perceived usefulness, perceived barriers to use, ease of use, and personal innovativeness. We additionally measured perceptions of social media across four dimensions: a waste of time/an essential use of time, very risky/very beneficial, very boring/very engaging. We included Likert-based ad-hoc items related to decision making, perceived risk, and professionalism. Additionally, we included free-text questions asking about general perceptions of online patient-surgeon communication and the look and feel of a potential new platform.
Analysis
We analyzed survey results using both qualitative and quantitative methods. Individuals who did not complete >80% of the survey and took less than 1 minute to complete the survey were not included in the analysis. Subscales were summed for scoring. Descriptive statistics were performed on demographic information and Likert-based scales. To identify characteristics associated with perceptions of social media use, nonparametric bivariate analysis was performed. Further, logistic and ordinal regression was used to characterize variables associated with the odds of thinking a new platform is needed and future use (Table 5–6). Of note, we utilized the term “gender minority” in analysis to represent women and gender diverse individuals due to limitations in sample size in these populations. Individuals with these identities are underrepresented in surgical specialties in medicine (C. L. Bennett et al. 2020; Ellis and Khubchandani 2021). We performed all statistical analysis using Stata 17.0 (Statacorp LLC, College Town TX).
Free-text entries were analyzed through an iterative qualitative coding process. First, four team members open coded the free text responses. They then met to discuss the patterns they saw in the data. The group used Miro to sort codes and build consensus on a codebook. The codebook was then applied to the free text by four members of the research team who then met to discuss discrepancies and find consensus.
Results
Participant Demographics and Characteristics
A total of N = 55 participants successfully completed the survey (response rate = 12%, Figure 1). Table 1 details participant demographics and characteristics. The mean age of participants was 47.9 (SD = 11.9). Participants were 56% men (n = 31), 42% women (n = 23), and 2% gender diverse (n = 1). Participants were primarily non-Hispanic white (52.7%) and Asian (21.8%). Participants were primarily from the US (n = 52, 94%) and practiced in 23 different states; the remainder were from Canada. Plastic surgeons (60%), urologists (18%), and gynecologists (15%) were represented in this sample, with 47% in academic practices and 38% in private practice. The median practice length was 6–10 years, but the most prevalent practice length was more than 21 years (35%). Participants performed a variety of gender-affirming procedures, with an average of 44% (SD = 35.2) of their practice consisting of gender-affirming surgery. On average, participants reported that 63.9% (SD = 31.5) of the gender-affirming surgery counseling they do with patients could be done in an online setting.
Social Media Use Patterns Amongst Surgeons
Participants used a median of 3 (interquartile range [IQR] 2–5) social media platforms for personal use and 2 (IQR 0–3) for professional use. Most participants used social media daily for personal use (n = 34, 62%) with the top platforms being Facebook and Instagram (Figure 2). Only 20% of participants (n = 11) reported daily use for professional purposes, with 31% (n = 17) reporting no professional social media use. Approximately one-quarter (n = 13, 24%) reported using social media to communicate with patients. Participants responded low on the frequency of use scale (median score = 5, IQR 3–9, max score 21).
General Views of Social Media
[Participants had a variety of perspectives on the role of social media use in their practice and communication with patients undergoing gender-affirming surgery. While median perceptions of social media measured through varying dimensions were neutral (waste of time/essential use of time median = 4, IQR = 3–5; very boring/very engaging mean = 4, IQR = 4–5; a bad/good way to communicate median = 4, IQR = 3–5; risky/beneficial median = 4, IQR = 2–5; see Table 2 and Figure 3), there was wide variation. Similarly, median responses were neutral to ad-hoc statements: “physicians should participate in social media with patients” (median = 4, IQR = 2–5; see Table 2 and Figure 4) and “patients talking about surgery online does more harm than good” (reverse-scored, median = 4, IQR = 2–5; see Table 2 and Figure 4), with variation in sentiments.]{.mark}
Perceptions of a Possible Platform Facilitating Patient-Surgeon Communication
Overall, surgeon support for a new platform for communication with patients was low, with 67% (n = 37) of participants saying that another platform was not needed. Hypothetical use of a new platform was variable, with 31% (n = 17) of participants noting they would use a new platform daily or multiple days a week and 28% (n = 15) saying they would never use one if it existed. The generally negative sentiment about a new platform was supported by free-text responses to the question “Are there any other thoughts regarding social media use and communication with patients online?” Out of 24 participants who provided free-text responses, 11 (46%) were coded as viewing a new platform as negative, 14 (58%) as neutral, and only 8 (33%) as positive. (Percentages add up to greater than 100% because responses could be coded in more than one category.)
In bivariate analysis, age, gender, specialty, or social media use constructs were not associated with feeling a new social media platform was necessary (Table 3). Frequency of social media use, perceived usefulness, and innovativeness was associated with perceived future use of a new platform (Table 4). In multivariate logistic regression adjusting for age, gender, and construct measurements, practice type was associated with thinking a new platform is needed. Individuals in private practice were 16 times more likely to think that a new platform is needed than individuals who work in an academic setting (p = .03; see Table 5). Specialty type, frequency of social media use, age, and gender did not impact odds of thinking a new platform is needed. In ordinal regression adjusting for age, gender, practice type, and social media constructs statistically significant in bivariate analysis, participants reporting a new social media platform is necessary were 6 times more likely to say they would use a platform more often if it existed compared to those who did not want a new platform (p = .006; see Table 6).
Though most surgeons did not support the idea of a new platform, participants did provide feedback on what features they would want to see in a new platform if it did exist. Protections for privacy and confidentiality was the most commonly mentioned feature, followed by opportunities to share photographs, video, and other media. There was disagreement on whether a platform should have a one-on-one chat function between surgeons and patients. Some stated that one-on-one chat would help preserve privacy and confidentiality, and others stated that one-on-one communication with patients should be restricted to a platform like EPIC, while a social media platform should only be used to communicate with patients more broadly.
Negative Implications of a New Platform Facilitating Patient-Surgeon Communication
Quantitative analysis demonstrated widespread perceived risk of social media use for gender-affirming surgeons. When asked to rank social media on a 1 to 7 Likert scale of very risky to very beneficial, the average score was 3.5 (SD = 1.7). Free-text responses supported this, with responses mentioning a variety of potential risks to both patients and surgeons (Figure 4).
Risk to Patients
The most cited risks to patients of a new social media platform were misinformation and liability (Figure 6). Some participants worried that misinformation could be spread to patients as a result of surgeons trying to “sell themselves” and their brands:
The key is to provide accurate information. There are too many videos of providers “selling” themselves—talking about how amazing they are with so few complications. In the end, patients want reliable information. Many, and perhaps a majority of patients, want surgeons to tell them what they need to hear and not what they want to hear. A social media platform that allows the dissemination of real information regarding gender surgery would be helpful for providers and for patients. (ID43)
Participant 43 felt that the current pressures on gender-affirming surgeons to self-promote and tell patients “what they want to hear” (ID43) via social media is a major contributor to the spread of misinformation to patients.
Regarding liability, participants were particularly concerned about how interacting with patients via social media could be done in ways protecting patients’ privacy and safety. One participant stated, “It’s a great tool but there has to be a line with how much medical advice can be given without getting into legal issues” (ID40). A related aspect of liability is the risk that patients would attempt to utilize a social media platform in emergency situations: “This is another way that patients in emergencies will communicate instead of calling, leading to delays of treatment and possible patient injuries” (ID49). This concern highlights the need for explicit boundaries in any new platform used for communication between surgeons and patients, making clear that communication on the platform should not be taken as individualized medical advice and that, if a patient is experiencing a health emergency, they should seek emergency treatment.
Risk to Surgeons
The most commonly cited risk to surgeons of a new social media platform was the additional burden that using such a platform would place on them. Participants mentioned the burden that a new platform would place on their time, which is already extremely limited.
It’s easier for me to just see patients. It’s easier for me to talk to patients. I’m already serving as my own transcriptionist dictating notes or hand typing them in an EMR. To be honest, last thing I want is more typing and uploading photos/videos. Just don’t have extra time for that. I am busy being a surgeon. I’d like to continue to be efficient, that’s the biggest hurdle. If I wasn’t busy, then yes, I understand patients select their surgeon based more on social media these days rather than where that person trained or experience. (ID37)
Concerns about surgeons’ already-limited time were enhanced by concerns about duplication of work between electronic medical records like EPIC and a potential new platform. Other responses mentioned closely related issues such as constant availability, burnout, and encroachment on personal life.
So many reasons to not normalize physician interactions via social media with patients. As it is, work creeps into the rest of life, this is just another example of how physician time is less respected than other professions, and part of it is our own doing by being excessively available. (ID46)
Participant 46 compared the amount of respect that physicians’ time commands to that of other professions to emphasize the burden of work encroaching on physicians’ personal lives. Others brought up the issue that physicians could not be compensated for time they put into communicating via social media:
I think in medical systems that have effective and convenient ways for patients to communicate with their physicians (through EPIC, virtual visits), adding means of communication through social media adds unnecessary burden to the physician. It can contribute to physician burnout if physicians cannot be compensated for their work through social media and need to find time on top of their normal workload to keep up. (ID27)
Several individuals also described concerns about what additional social media use would mean for surgeon identity and culture, with specific concerns about how social media could change the doctor-patient relationship and medical professionalism. One participant stated that social media use “does a disservice to our core message of thoughtful, personal care” (ID15). Another stated: “I don’t think it is unethical to use social media, but it kind of cheapens the doctor patient relationships to me. Doctors who rely on it too much seem a little desperate” (ID53).
Finally, participants had concerns about online mistreatment and their safety if they were to engage publicly in social media:
Because social media lends to anonymity in some cases, it may allow some people to remain behind the screen and communicate without keeping in mind that it's a real person on the other end. While patients are vulnerable, physicians can be vulnerable too. When physicians are vulnerable, they are often treated as if accepting abuse and microaggressions is part of being empathetic - this should be avoided. (ID27)
In some cases, these concerns were related to the current sociopolitical contexts of the states in which they practice medicine. One described the dangers of surgeons’ social media use in states with recent restrictions on gender-affirming care as follows:
Social media for gender affirmation surgeons is dangerous. I live and practice in [state], and the state house increasingly is introducing bills to try to limit gender affirming care. There is also a dangerous rhetoric among the right wing in [state]that conflates providing gender affirming care, especially in those who are not yet the age of majority, with grooming and pedophilia. It is an especially fraught time for physicians who try to provide best care and follow the best practice guidelines. (ID57)
Social media use can increase physicians’ vulnerability to harassment. The very real risks of abuse and harassment, in addition to increased demands on surgeons’ time, must be seriously considered in designing a patient-surgeon communication platform.
Positive Implications of a New Platform Facilitating Patient-Surgeon Communication
Despite overall support for a new platform being low, qualitative analysis of free-text responses also revealed potential positive implications of a new social media platform for patient-surgeon communication. Positive implications included improvements to patient education and patient care. Participants emphasized balancing risks and benefits of social media use.
Improve Patient Education
Participants reported that social media can contribute to patient education, with a median score of 5 (out of a possible 7) in response to the ad-hoc statement “Social media can be an effective tool for patient education.” Free-text responses that mentioned patient education described social media as “a critical tool for education and relaying accurate information” (ID:13). Another participant stated: “A social media platform that allows the dissemination of real information regarding gender surgery would be helpful for providers and for patients” (ID43; Figure 5).
Enhance Patient Care
Participants also answered that social media can contribute in a positive way to surgical decision-making, with a median score of 5 (out of a possible 7) in response to the ad-hoc statement “Discussions on social media can help patients make decisions about surgery” (Figure 5). While no free-text responses explicitly mentioned surgical decision-making, participants did state that social media could have positive implications for patient care. For example, one participant acknowledged that social media is a difficult arena to navigate but that “done correctly, it should enhance patient care” (ID11).
Balancing Risks and Benefits
Most of the free-text responses that mentioned positive implications of social media simultaneously mentioned negative implications. Balancing risks and benefits was explicitly mentioned in several free text responses. One participant stated that there is a “fine line between education in a relatable manner and poor taste and ominous implications” (ID15). Another participant elaborated further on those potentially “ominous implications”:
I would love to harvest the benefits of social media interaction without the constant risk of over-reaction, being misunderstood despite all efforts, inappropriate contact outside of the app, etc. (ID59)
These responses highlight how a platform for patient-surgeon communication might improve patient education and enhance patient care, while at the same time ensuring that these benefits outweigh the risks mentioned in the previous section.
Discussion
We investigated gender-affirming surgeons’ attitudes toward an online platform designed to facilitate communication with trans patients considering surgery using both qualitative and quantitative methods. Our findings demonstrate that surgeons perceived communicating with patients via social media to be risky to both patients and surgeons. This is in line with other literature showing that physicians are concerned about compliance with HIPAA and unsure of their ethical and legal obligations when communicating with patients online (Brown, Ryan, and Harris 2014; Ventola 2014).
Given the lack of enthusiasm that most participants in this study had for using social media as a tool for communicating with trans patients about gender-affirming surgery, this raises the question of how necessary or even possible it is to have surgeons in online spaces. The necessity has been established by earlier research demonstrating that trans users in online spaces such as Reddit and Transbucket desire more participation from surgeons to increase accuracy and reduce misinformation (Augustaitis et al. 2021; Chuanromanee et al. 2021). A key issue that this earlier research has raised is the difficulty of flagging inaccurate content, demonstrating a need for improved content moderation to ensure that the information trans patients are receiving through online platforms is both correct and current. Some level of surgeon involvement in these platforms could help to ameliorate these issues. There is a growing body of evidence that online patient-physician communication can benefit both groups in myriad ways including increasing patients’ understanding of medical information, strengthening the emotional connection between doctors and their patients, and building physicians’ professional capital (e.g. online reputation and demand for their services) (Lu and Zhang 2019; Qiao, Yan, Wang 2021). These findings demonstrate that physician engagement in online patient communities is not only possible but can be beneficial to both parties.
Many surgeons in this study were aware of the unique constraints involved with communicating with prospective patients about gender-affirming surgery, particularly as they relate to the current sociopolitical climate in which many gender-affirming surgeons receive personal threats to their safety or their ability to do their work is threatened by anti-trans legislation (O’Reilly 2021). Based on our findings, surgeons who would otherwise be more willing to participate in an online patient communication platform may be deterred by the current cultural and political climate. There is evidence that having healthcare providers or health educators involved in an online community focused on sexual health and HIV prevention for Black men who have sex with men was critical in reducing misinformation and helping to moderate conversations around health stigma (Blackburn et al. 2021). This evidence of the positive impact of having health care workers involved in an online community focused on other highly stigmatized and politicized health topics should be reassuring to gender-affirming surgeons who have a desire to participate in online patient communication spaces but worry about what impact they might have in these communities.
Most participants did not think a new platform was needed despite the fact that many of the concerns participants had about online communication with patients were related to technical elements that could be ameliorated with thoughtful design of a new platform that incorporated solutions to these concerns. Surgeons in our study described several technical factors that would need to be present in a social media platform designed for communicating with patients about gender-affirming surgery, including a Q&A feature, options for one-on-one communication with patients, and integration with existing EMR platforms. A more complex element that surgeons felt was essential was the ability to maintain patients’ privacy and confidentiality in a manner that is compliant with HIPAA. In addition to concerns about patient safety as it relates to privacy and confidentiality, participants were also concerned about surgeons’ safety in an online environment. Some had previous experiences with online abuse and harassment making them hesitant to interact with patients via social media, while others feared negative online interactions given the political climate surrounding gender-affirming surgery today. To balance trans patients’ desires for more surgeon involvement in social media platforms discussing gender-affirming surgery with the elements that surgeons in this study identified as necessary for their participation in such a platform, careful attention to both the technical and ethical aspects of platform development are required (Huh 2015; Huh and Pratt 2014).
Some surgeons in our study felt that social media could have positive implications for patient care if harnessed correctly, especially those who seemed to have an awareness of the historical importance of online spaces for trans individuals sharing and seeking information regarding gender-affirming health care. Yet even participants who reported current online engagement with patients were hesitant to fully embrace an online communication platform given personal negative experiences they have had when attempting to discuss gender-affirming surgery with patients in online spaces. To harness positive aspects, a new platform could contain a dedicated space for individual surgeons to make standardized information available to potential patients that would normally be given through a consultation, which participants indicated was over 60% of time spent in consultation. When patients did have formal consultations with surgeons, then, they could already have accessed the general information that takes up considerable time during a visit. The time during the consultation could be spent on discussing aspects of the procedure specific to that individual patient, ultimately leading to higher quality and possibly shorter consultation visits. Because compensation for time spent on consultations is lower than for time spent on procedures (Reid et al. 2022), reducing the time spent on consultation could be an incentive for surgeons to utilize this type of platform. Further, having content available online would allow patients to access information about techniques offered and medical requirements directly from surgeons, leading to more informed decision-making for patients seeking consultations. This could potentially lead to a higher rate of surgical procedures booked per consultation for surgical teams. For patients, this could ultimately reduce the time, travel, and financial burdens in the process of receiving gender-affirming surgery.
Additionally, a platform dedicated to facilitating surgeon-patient communication could support surgeons’ participation by directly compensating surgeons for the time they spent on the platform. While it might only be possible to financially compensate a very small number of surgeons for a limited number of hours, this would still be an improvement on the current social media landscape and would ensure that there was at least some amount of surgeon oversight to help mitigate the spread of misinformation about gender-affirming procedures. Alternatively, surgical residency programs could require residents to spend a certain amount of time in online spaces with patients providing information, answering questions, and combating misinformation through patient portal responses (though this would require appropriate supervision to ensure information quality and would have to be balanced with other demands on trainees’ time). While telemedicine and the use of online messaging has exploded since the pandemic, residents and medical students receive very little training on these types of interactions.
This study’s results indicate that gender-affirming surgeons have relatively little interest in participating in a newly developed platform facilitating communication with potential patients; however, many of the reasons participants gave for not being interested could be addressed through the measures described here. A solution that would both address surgeons’ concerns and fulfill patients’ unmet needs could be a platform where individual surgeons or groups could make standardized information about the gender-affirming procedures they provide available to potential patients to reduce the portion of time spent on standardized information sharing during consultations. The platform could contain a private messaging feature for prospective patients to ask surgeons questions, and each surgeon using the platform could dedicate a limited number of hours each week to responding to patient questions with appropriate compensation. These interactions would very explicitly not be medical advice and users of the platform would need to sign agreements stating that they understood this to address surgeons’ concerns about liability. To provide some level of surgeon compensation while maintaining accessibility for potential patients, one solution could be two versions of the platform: a free version where users would access standardized information on gender-affirming procedures, and a paid version that allowed users to interact directly with surgeons. Future studies should assess surgeons’ willingness to participate in a platform that included the features identified as essential by participants in this study.
One limitation of this study is the response rate of only 12%. This could be related to our survey distribution method, wherein we contacted surgeons at the email addresses listed publicly on the WPATH member directory and transhealth.org, which may or may not be checked frequently. This response rate could further reflect the enthusiasm of this population for social media, and a reflection of their limited time. Further, using the WPATH member directory and transhealth.org to identify gender affirming surgeons is a limitation in and of itself. Some surgeons who perform gender-affirming care as part of their clinical work are not members of WPATH and have not taken the steps needed to be listed as a gender-affirming surgeon on transhealth.org. These surgeons were not captured in recruitment for this study and as such some degree of selection bias influenced the composition of the final sample.
While we attempted to utilize validated measures to assess social media use and attitudes, there are few instruments available. Another limitation is that participants’ responses were shaped by their own interpretations of the term “social media.” Some participants seemed to be thinking of social media only as a community-facing advertising method (e.g., a surgeon page on Facebook), whereas others were thinking of platforms that allow for community members to communicate and share information with each other (e.g., reddit, Transbucket).
Conclusion
There will always be some risk inherent to communication between surgeons and patients via social media. Threats to privacy and confidentiality are not always predictable or preventable, though any platform developed in the future would make protecting the safety of all users a top priority. As participants in this study stated, using social media is about balancing risks and benefits. An online communication platform for patients and surgeons could provide important benefits, such as disseminating accurate information and mitigating misinformation about gender-affirming surgery for potential patients and improving patient care. Thus, developing an online platform facilitating communication between gender-affirming surgeons and patients is worthy of further study.
References
Augustaitis, Laima, Leland A. Merrill, Kristi E Gamarel, and Oliver L. Haimson. 2021. “Online Transgender Health Information Seeking: Facilitators, Barriers, and Future Directions.” In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, 1–14. Yokohama: ACM. https://doi.org/10.1145/3411764.3445091.
Bennett, Christopher L., Olesya Baker, Erika L. Rangel, and Regan H. Marsh. 2020. “The Gender Gap in Surgical Residencies.” JAMA Surgery 155 (9): 893. https://doi.org/10.1001/jamasurg.2020.2171.
Bennett, Katelyn G., Nicholas L. Berlin, Mark P. MacEachern, Steven R. Buchman, B. Aviva Preminger, and Christian J. Vercler. 2018. “The Ethical and Professional Use of Social Media in Surgery: A Systematic Review of the Literature.” Plastic and Reconstructive Surgery 142 (3): 388e–98. https://doi.org/10.1097/PRS.0000000000004692.
Blackburn, Natalie A., Willa Dong, Megan Threats, Megan Barry, Sara LeGrand, Lisa B. Hightow-Weidman, Karina Soni, Deren V. Pulley, Jose A. Bauermeister, and Kate Muessig. 2021. “Building Community in the HIV Online Intervention Space: Lessons From the HealthMPowerment Intervention.” Health Education & Behavior 48 (5): 604–14. https://doi.org/10.1177/10901981211003859.
Blotner, Charlie, and Micah Rajunov. 2018. “Engaging Transgender Patients: Using Social Media to Inform Medical Practice and Research in Transgender Health.” Transgender Health 3 (1): 225–28. https://doi.org/10.1089/trgh.2017.0039.
Brown, James, Christopher Ryan, and Anthony Harris. 2014. “How Doctors View and Use Social Media: A National Survey.” Journal of Medical Internet Research 16 (12): e267. https://doi.org/10.2196/jmir.3589.
Chuanromanee, Tee, and Ronald Metoyer. 2021. “Transgender People’s Technology Needs to Support Health and Transition.” In Proceedings of the 2021 CHI Conference on Human Factors in Computing Systems, 1–13. Yokohama: ACM. https://doi.org/10.1145/3411764.3445276.
Darwin, Helana. 2017. “Doing Gender Beyond the Binary: A Virtual Ethnography.” Symbolic Interaction 40 (3): 317–34. https://doi.org/10.1002/symb.316.
De La Cruz Monroy, Martha F. I., and Afshin Mosahebi. 2019. “The Use of Smartphone Applications (Apps) for Enhancing Communication With Surgical Patients: A Systematic Review of the Literature.” Surgical Innovation 26 (2): 244–59. https://doi.org/10.1177/1553350618819517.
Ellis, Danielle I., and Jasmine A. Khubchandani. 2021. “The State of Diversity in American Surgery: A Call to Action.” Annals of Surgery 273 (1): e3–4. https://doi.org/10.1097/SLA.0000000000004518.
Eysenbach, G. 2003. “The Impact of the Internet on Cancer Outcomes.” CA: A Cancer Journal for Clinicians 53 (6): 356–71. https://doi.org/10.3322/canjclin.53.6.356.
Gustafson, David H., Robert Hawkins, Suzanne Pingree, Fiona McTavish, Neeraj K. Arora, John Mendenhall, David F. Cella, et al. 2001. “Effect of Computer Support on Younger Women with Breast Cancer.” Journal of General Internal Medicine 16 (7): 435–45. https://doi.org/10.1046/j.1525-1497.2001.016007435.x.
Haimson, Oliver L., Justin Buss, Zu Weinger, Denny L. Starks, Dykee Gorrell, and Briar Sweetbriar Baron. 2020. “Trans Time: Safety, Privacy, and Content Warnings on a Transgender-Specific Social Media Site.” Proceedings of the ACM on Human-Computer Interaction 4 (CSCW2): 1–27. https://doi.org/10.1145/3415195.
Hartzler, Andrea, and Wanda Pratt. 2011. “Managing the Personal Side of Health: How Patient Expertise Differs from the Expertise of Clinicians.” Journal of Medical Internet Research 13 (3): e62. https://doi.org/10.2196/jmir.1728.
Huh, Jina. 2015. “Clinical Questions in Online Health Communities: The Case of ‘See Your Doctor’ Threads.” In Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing, 1488–99. Vancouver: ACM. https://doi.org/10.1145/2675133.2675259.
Huh, Jina, David W McDonald, Andrea Hartzler, and Wanda Pratt. 2013. “Patient Moderator Interaction in Online Health Communities.” AMIA Annual Symposium Proceedings 2013: 627–36.
Huh, Jina, and Wanda Pratt. 2014. “Weaving Clinical Expertise in Online Health Communities.” In Proceedings of the SIGCHI Conference on Human Factors in Computing Systems, 1355–64. Toronto: ACM. https://doi.org/10.1145/2556288.2557293.
Kim, Hyang-Sook, and Amy Mrotek. 2016. “A Functional and Structural Diagnosis of Online Health Communities Sustainability: A Focus on Resource Richness and Site Design Features.” Computers in Human Behavior 63: 362–72. https://doi.org/10.1016/j.chb.2016.05.004.
Kim, Hyang-Sook, and S. Shyam Sundar. 2014. “Can Online Buddies and Bandwagon Cues Enhance User Participation in Online Health Communities?” Computers in Human Behavior 37: 319–33. https://doi.org/10.1016/j.chb.2014.04.039.
Lo, Brian, Rebecca Charow, Sarah Laberge, Vasiliki Bakas, Laura Williams, and David Wiljer. 2022. “Why Are Patient Portals Important in the Age of COVID-19? Reflecting on Patient and Team Experiences From a Toronto Hospital Network.” Journal of Patient Experience 9: 237437352211122. https://doi.org/10.1177/23743735221112216.
Lu X, Zhang R. 2019. “Impact of Physician-Patient Communication in Online Health Communities on Patient Compliance: Cross-Sectional Questionnaire Study.” Journal of Medical Internet Research 21 (5): e12891. https://doi.org/10.2196/12891.
Ma, Xiumei, Pengfei Zhang, Fanbo Meng, and Kee-hung Lai. 2022. “How Does Physicians’ Educational Knowledge-Sharing Influence Patients’ Engagement? An Empirical Examination in Online Health Communities.” Frontiers in Public Health 10: 1036332. https://doi.org/10.3389/fpubh.2022.1036332.
Maisner, Rose S., Kailash Kapadia, Ryan Berlin, and Edward S. Lee. 2023. “Is #Gender Affirmation Surgery Trending? An Analysis of Plastic Surgery Residency Social Media Content.” Transgender Health, published ahead of print, February 14, 2023. http://doi.org/10.1089/trgh.2021.0215.
McGowan, Brian, Molly Wasko, Bryan Steven Vartabedian, Robert Miller, Freiherr, and Maziar Abdolrasulnia. 2012. “Understanding the Factors That Influence the Adoption and Meaningful Use of Social Media by Physicians to Share Medical Information.” Journal of Medical Internet Research 14 (5): e117. https://doi.org/10.2196/jmir.2138.
Mehrotra, Ateev, Kristin Ray, Diane Brockmeyer, Michael Barnett, and Jessica Anne Bender. 2020. “Rapidly Converting to ‘Virtual Practices’: Outpatient Care in the Era of COVID-19.” American Telemedicine Association, April 28, 2020. https://www.americantelemed.org/resources/rapidly-converting-to-virtual-practices-outpatient-care-during-covid-19/.
Nath, Chinmoy, Jina Huh, Abhishek Kalyan Adupa, and Siddhartha R Jonnalagadda. 2016. “Website Sharing in Online Health Communities: A Descriptive Analysis.” Journal of Medical Internet Research 18 (1): e11. https://doi.org/10.2196/jmir.5237.
O’Reilly, Kevin B. 2021. “Why Anti-Transgender Bills are a Dangerous Intrusion on Medicine.” American Medical Association, May 7, 2021. https://www.ama-assn.org/delivering-care/population-care/why-anti-transgender-bills-are-dangerous-intrusion-medicine.
Qiao, Wanxin, Zhijun Yan, and Xiaohan Wang. 2021. “Join or Not: The Impact of Physicians’ Group Joining Behavior on Their Online Demand and Reputation in Online Health Communities.” Information Processing & Management 58 (5): 102634. https://doi.org/10.1016/j.ipm.2021.102634.
Reid, Rachel O., Ashlyn K. Tom, Rachel M. Ross, Erin L. Duffy, and Cheryl L. Damberg. 2022. “Physician Compensation Arrangements and Financial Performance Incentives in US Health Systems.” JAMA Health Forum 3 (1): e214634. https://doi.org/10.1001/jamahealthforum.2021.4634.
Robinson, Jamie R., Alissa Valentine, Cathy Carney, Daniel Fabbri, and Gretchen P. Jackson. 2017. “Complexity of Medical Decision-Making in Care Provided by Surgeons through Patient Portals.” Journal of Surgical Research 214: 93–101. https://doi.org/10.1016/j.jss.2017.02.077.
Scalia, Peter, Katherine M. Tighe, Glyn Elwyn, Pamela J. Bagley, Heather B. Blunt, Benjamin Boh, Oakland C. Walters, and Rachel A. Moses. 2021. “A Systematic Review of Decision Aids for Gender Affirming Therapy.” Translational Andrology and Urology 10 (6): 2574–82. https://doi.org/10.21037/tau-20-1000.
Song, Siyou, Keon Min Park, Kiet Phong, and Esther A. Kim. 2022. “Evaluating the Quality and Reliability of Gender-Affirming Surgery Videos on YouTube and TikTok.” Plastic and Reconstructive Surgery – Global Open 10 (7): e4443. https://doi.org/10.1097/GOX.0000000000004443.
Stewart, Jeffrey J, Islam Fayed, Shawnda Henault, Babak Kalantar, and Jean-Marc Voyadzis. 2019. “Use of a Smartphone Application for Spine Surgery Improves Patient Adherence with Preoperative Instructions and Decreases Last-Minute Surgery Cancellations.” Cureus 11 (3): e4192. https://doi.org/10.7759/cureus.4192.
Stork, Brian Robert. 2023. “The Influence of Social Medial Influencers on Urology Information: Where Are All the Urologists?” Société Internationale d’Urologie Journal 4 (2): 125–26.
Ventola, C Lee. 2014. “Social Media and Health Care Professionals: Benefits, Risks, and Best Practices.” Pharmacy and Therapeutics 39 (7): 491–520.
Yeadon-Lee, Tracey. 2016. “What’s the Story? Exploring Online Narratives of Non-Binary Gender Identities.” The International Journal of Interdisciplinary Social and Community Studies 11 (2): 19–34.
Zarefsky, Marc. 2023. “What’s Adding to Doctor Burnout? Check Your Patient Portal Inbox.” American Medical Association, February 3, 2023. https://www.ama-assn.org/practice-management/digital/what-s-adding-doctor-burnout-check-your-patient-portal-inbox.
Zhang, Xin, Shanzhen Gao, Yanyan Cheng, and Fanbo Meng. 2022. “Encouraging Physicians’ Continuous Knowledge-Sharing in Online Health Communities: A Motivational Perspective.” Frontiers in Public Health 10: 1036366. https://doi.org/10.3389/fpubh.2022.1036366.
Acknowledgments
Funding: University of Michigan's Institute for Research on Women and Gender (IRWG) Faculty Seed Grant.
Table 1. Participant Demographics (N = 55)
| Characteristic | M (SD) / n (%) |
|---|---|
| Age | 47.9 (11.9) |
| Gender | |
| Male | 31 (56.4) |
| Female | 23 (41.8) |
| Gender diverse | 1 (1.8) |
| Race | |
| White/Caucasian non-Hispanic | 29 (52.7) |
| Black/African American non-Hispanic | 2 (3.6) |
| Asian non-Hispanic | 12 (21.8) |
| White Hispanic | 3 (5.5) |
| Middle Eastern | 1 (1.8) |
| Native American | 1 (1.8) |
| Pacific Islander | 1 (1.8) |
| Multiracial | 3 (5.5) |
| Other | 1 (1.8) |
| N/A | 2 (3.6) |
| Country | |
| USA | 52 (94.6) |
| Canada | 3 (5.5) |
| Specialty | |
| Plastic surgery | 33 (60.0) |
| Urology | 10 (18.2) |
| Obstetrics and gynecology | 8 (14.6) |
| Other | 4 (7.3) |
| Practice setting | |
| Academic | 26 (47.3) |
| Private practice | 21 (38.2) |
| Combination | 8 (14.6) |
| Practice length | |
| In training | 2 (3.6) |
| < 5 years | 12 (21.8) |
| 6–10 years | 15 (27.3) |
| 11–15 years | 6 (10.9) |
| 16–20 years | 1 (1.8) |
| 21+ years | 19 (34.6) |
| Procedures performed | |
| Chrondrolaryngoplasty | 16 (29.1) |
| Facial feminization | 17 (30.9) |
| Facial masculinization | 14 (25.5) |
| Hysterectomy | 8 (14.6) |
| Orchiectomy | 18 (32.7) |
| Penectomy w/o genital reconstruction | 9 (16.4) |
| Metoidioplasty | 16 (29.1) |
| Phalloplasty | 15 (27.3) |
| Vaginoplasty | 13 (23.6) |
| Zero-depth vaginoplasty/labiaplasty | 18 (32.7) |
| Other | 5 (9.1) |
| Mean percent of practice is GAS | 44.1 (35.2) |
| Percent of GAS consultation standardized | 66.7 (35.6) |
| Percent of GAS counseling that could be done online | 63.9 (31.5) |
Table 2. Construct, Ad-Hoc, and Dimension Scores (N = 55)
| Measures | Median Score (IQR) |
|---|---|
| Construct | |
| Frequency of social media use (3–21, lower is less frequent) | 5 (3–9) |
| Usefulness (5–35, higher is more useful) | 14 (9–22) |
| Ease of use (3–21, higher is higher perceived ease of use) | 15 (10–17) |
| Personal innovativeness (2–14, higher is higher innovativeness) | 6 (4–8) |
| Barriers to use (3–21, higher is higher barriers) | 13 (10–15) |
| Ad-hoc statements | |
| Social media can be an effective tool for patient education | 5 (5–6) |
| Physicians should participate in social media with patients | 4 (2–5) |
| Patients talking about surgery online does more harm than good (reverse coded) | 4 (2–5) |
| Discussions on social media can help patients make decisions about surgery | 5 (4–6) |
| Physicians who talk to patients on social media are unprofessional | 3 (2–4) |
| Social media dimensions | |
| A waste of time (1) – an essential use of time (7) | 4 (3–5) |
| Very risky (1) – very beneficial (7) | 4 (2–5) |
| Very boring (1) – very engaging (7) | 4 (4–5) |
| A bad way to communicate current info (1) – a great way to communicate current info (7) | 4 (3–5) |
| Note. Scores presented as medians and interquartile ranges given the low sample size and Likert-based scoring. |
Table 3. Need for New Platform Stratified by Demographics and Construct Scores (N = 55)
| Characteristic | Yes | No | p |
|---|---|---|---|
| Agea | |||
| < 40 | 7 (36.8) | 12 (63.2) | .94 |
| 40–60 | 8 (32.0) | 17 (68.0) | |
| > 60 | 3 (33.3) | 6 (66.7) | |
| Gendera | |||
| Men | 9 (29.0) | 22 (71.0) | .51 |
| Gender minority† | 9 (37.5) | 15 (62.5) | |
| Specialtya | |||
| Plastic surgery | 11 (33.3) | 22 (66.7) | .98 |
| Urology | 3 (30.0) | 7 (70.0) | |
| Ob/Gyn and other | 4 (33.3) | 8 (66.7) | |
| Practice settinga | |||
| Academic | 6 (24.0) | 19 (76.0) | .10 |
| Private | 10 (47.6) | 11 (52.4) | |
| Combination | 1 (12.5) | 7 (87.5) | |
| Social media scalesb | |||
| Frequency of social media use | 6 (5–10) | 5 (3–9) | .36 |
| Usefulness | 17 (10–22) | 15 (8–20) | .40 |
| Ease of use | 14.5 (11–16) | 16 (10–17) | .39 |
| Barriers to use | 13.5 (12–16) | 13 (10–15) | .26 |
| Innovativeness | 6 (4–8) | 6 (4–8) | .55 |
| Note. a: Chi-square test utilized, bKruskall-Wallis test utilized, †includes women and gender diverse individuals |
Table 4. New Platform Use Stratified by Demographics and Construct Scores (N = 55)
| Characteristic | Daily | Multiple times a week | Weekly | Monthly | Every few months | Annually | Never | p |
|---|---|---|---|---|---|---|---|---|
| Agea | ||||||||
| < 40 | 0 (0) | 2 (11.1) | 4 (22.2) | 2 (11.1) | 3 (16.7) | 1 (5.6) | 6 (33.3) | .41 |
| 40–60 | 3 (12.5) | 7 (29.2) | 3 (12.5) | 2 (8.33) | 1 (4.2) | 1 (4.2) | 7 (29.2) | |
| > 60 | 0 (0) | 4 (44.4) | 3 (33.3) | 0 (0) | 0 (0) | 0 (0) | 2 (22.2) | |
| Gendera | ||||||||
| Men | 2 (6.5) | 10 (32.3) | 8 (25.8) | 2 (6.5) | 3 (9.7) | 2 (6.5) | 4 (12.9) | .10 |
| Gender minority† | 1 (4.4) | 4 (17.4) | 3 (13.0) | 3 (13.0) | 1 (4.4) | 0 (0) | 11 (47.8) | |
| Specialtya | ||||||||
| Plastic surgery | 1 (3.2) | 11 (35.5) | 5 (16.1) | 2 (6.5) | 2 (6.5) | 2 (6.5) | 8 (25.1) | .37 |
| Urology | 1 (10.0) | 1 (10.0) | 2 (20.0) | 0 (0) | 2 (20.0) | 0 (0) | 4 (40.0) | |
| Ob/Gyn and other | 1 (8.3) | 2 (16.7) | 3 (25.0) | 3 (25.0) | 0 (0) | 0 (0) | 3 (25.0) | |
| Practice settinga | ||||||||
| Academic | 1 (4.2) | 6 (25.0) | 3 (12.5) | 3 (12.5) | 3 (12.5) | 2 (8.3) | 6 (25.0) | .52 |
| Private | 1 (4.8) | 8 (38.1) | 5 (23.8) | 1 (4.8) | 0 (0) | 0 (0) | 6 (28.6) | |
| Combination | 1 (12.5) | 0 (0) | 2 (25.0) | 1 (12.5) | 1 (12.5) | 0 (0) | 3 (37.5) | |
| Social media scalesb | ||||||||
| Frequency of social media use | 9 (8–14) | 7 (5–9) | 7 (4–11) | 5 (3–5) | 7.5 (4–11.5) | 3.5 (3–4) | 5 (3–7) | .06 |
| Usefulness | 9 (5–18) | 20 (14–22) | 20 (15–29) | 9 (6–10) | 16.5 (10.5–26) | 7.5 (5–10) | 11 (5–15) | .02 |
| Ease of use | 16 (13–16) | 12 (8–15) | 14 (12–16) | 16 (6–16) | 11 (7.5–15) | 13.5 (8–19) | 17 (10–21) | .33 |
| Barriers to use | 14 (14–15) | 12.5 (10–14) | 13 (6–16) | 16 (15–17) | 16.5 (11–18) | 12 (11–13) | 13 (10–15) | .45 |
| Innovativeness | 11 (9–11) | 7 (4–8) | 6 (4–7) | 3 (3–4) | 6 (3–9) | 5.5 (4–7) | 5 (4–6) | .04 |
Figures
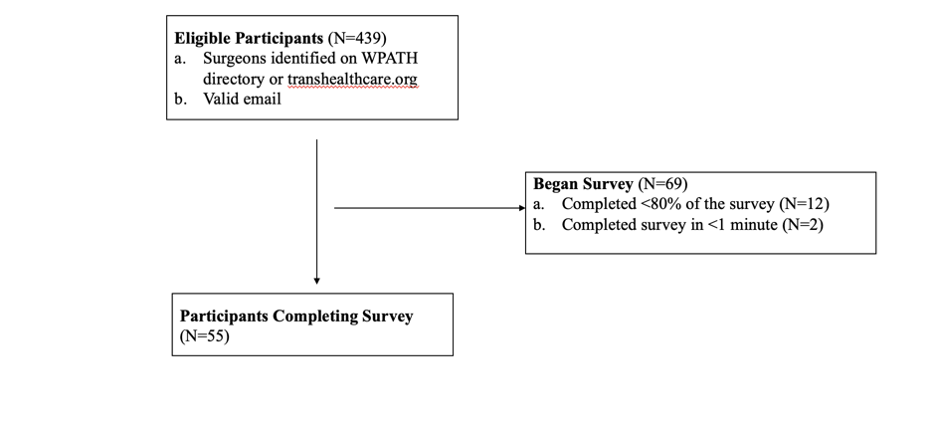
Figure 1. Eligibility criteria and participants
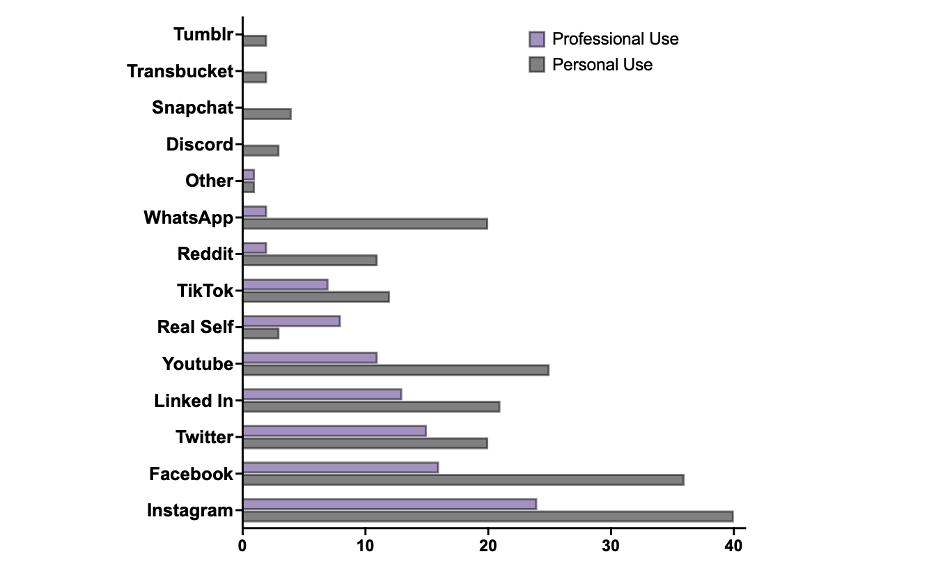
Figure 2. Number of surgeons using social media platforms for professional and personal use
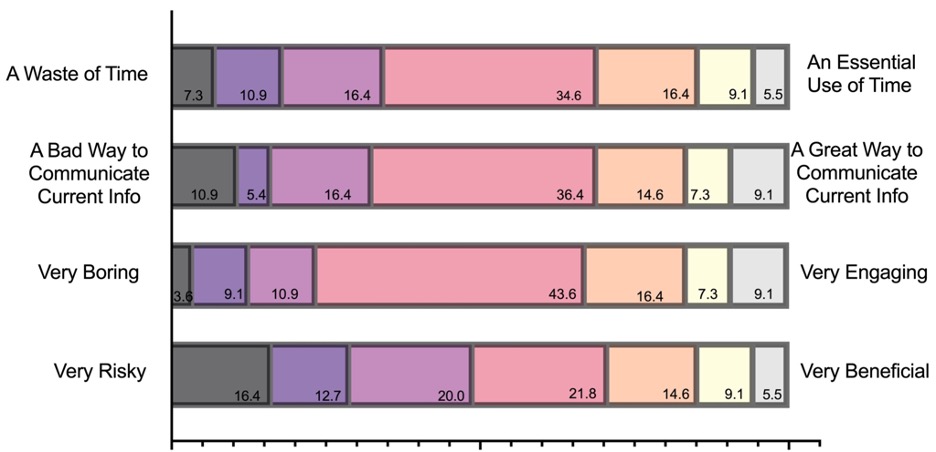
Figure 3. Dimensions of social media
Note. While median scores for dimensions suggest participants were indifferent about social media, the distribution of these scales varied, particularly for very risky/very beneficial.
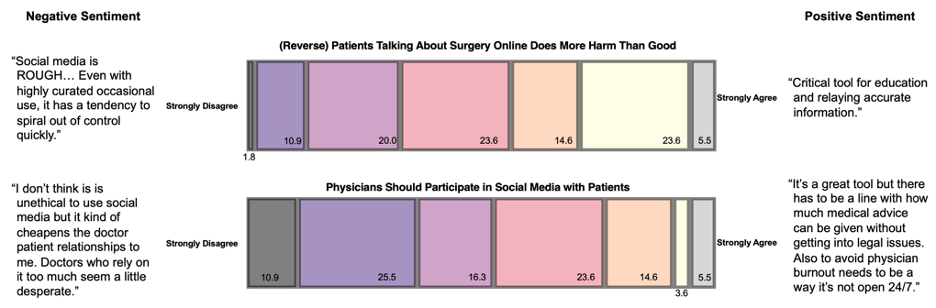
Figure 4. Joint display of general perceptions of social media
Note. While the median survey scores suggest surgeons were indifferent about social media and interacting with patients on these platforms, there was wide variation in scores, as well as free-text responses.
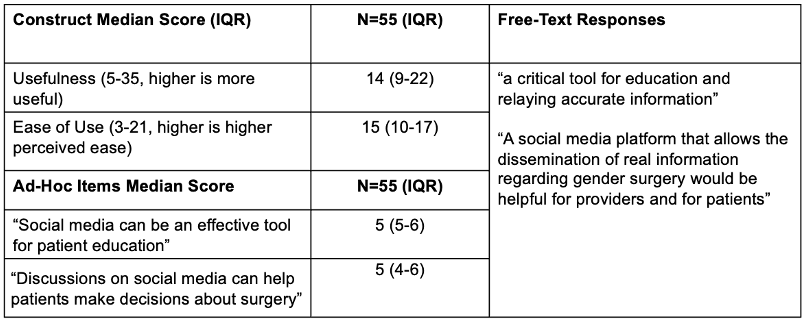
Figure 5. Joint display of positive implications for social media
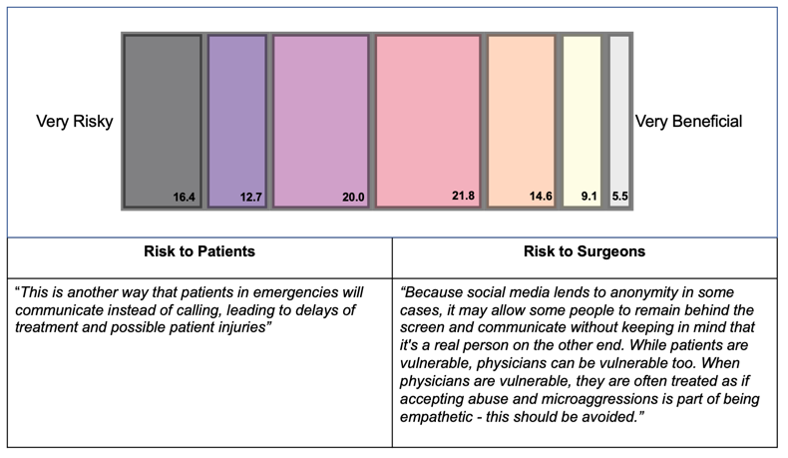
Figure 6. Joint display of negative implications for social media