Building a Rural Gynecology Gender Health Program to Bring Care Closer to Home
Julia S. Mead , Charlotte V. Hastings , Ilana Cass , Ella A. Damiano
Transgender and gender diverse patients face significant healthcare disparities that are often exacerbated for those living in rural areas. Our aim is to describe the characteristics of and medical services utilized by a transgender and gender diverse population seeking gynecologic care in a rural area. We conducted a retrospective chart review of transgender and gender diverse individuals who sought care and/or underwent gender-affirming gynecologic surgery at our institution. We compared patients presenting to the gynecology clinic from 2017–2018 to patients presenting to the dedicated Gynecology Gender Clinic from 2019–2020. We also describe the features that distinguish the clinic as specialized care. The clinic was able to utilize a pre-visit questionnaire to obtain patient name, pronouns, and gender identity in advance of the visit. Total unique patient volume increased by 83% (average 12 per year to average 22 per year). Hysterectomies performed increased by 320% (from 5 to 21 post-implementation) and encounter volume increased by 84%. The development of a Gynecology Gender Clinic program has led to an increase in clinical and surgical volume, improving access to care. Our data demonstrates feasibility of implementing the clinic and demand for specialized gender care in a rural community.
- Volume (Issue)
- 2(1-2)
- Published
- June 30, 2023
- DOI
- 10.57814/kp9j-p512
- Copyright
- © 2023. The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0)
- Preferred Citation
- Mead, Julia S., Hastings, Charlotte V., Cass, Ilana, Damiano, Ella A.. 2023. "Building a Rural Gynecology Gender Health Program to Bring Care Closer to Home." Bulletin of Applied Transgender Studies 2 (1-2): 107-118. https://doi.org/10.57814/kp9j-p512
Transgender individuals face significant healthcare disparities and barriers to care that are often exacerbated for those living in rural areas (Fantz 2014; Sinnard, Raines, and Budge 2016; Tinc et al. 2020). Multiple factors contribute to this disparity, including fear of discrimination, direct mistreatment, or refusal of care by providers or ancillary staff, as well as higher rates of uninsured or underinsured status (Fantz 2014; Bradford et al. 2013). Additionally, trans individuals living in rural areas may experience increased isolation and discrimination compared to urban populations, leading to further marginalization, reluctance to present for care, and decreased access to specialized clinics (Poteat, German, and Kerrigan 2013; Rowan et al. 2019; Whitehead, Shaver, and Stephenson 2016).
Several studies have demonstrated decreased primary care utilization, including vaccinations and cancer screening tests, amongst the rural transgender population, despite adequate insurance coverage. This may be due to a combination of barriers faced by rural populations in general (poor transportation infrastructure, low provider density), compounded by healthcare disparities specific to trans patients (outright discrimination, stigma, provider knowledge gaps; (American College of Obstetricians and Gynecologists 2014; Horvath et al. 2014). Additionally, transgender patients face greater travel distances to receive medical care (Stewart, Lee, and Damiano 2020; Whitehead, Shaver, and Stephenson 2016). The factors leading to increased distance travelled are myriad. For some patients, it may be a function of rurality and distance to a metropolitan area, especially for patients with an interest in receiving care from a knowledgeable provider with experience caring for trans individuals Berli et al. 2017). Other patients, especially those living in more remote or isolated areas, may fear breaches in their personal medical information when presenting for medical care, which can lead to further stigmatization and risks to personal safety (Harb et al. 2019; Logie et al. 2019; Whitehead, Shaver, and Stephenson 2016).
Population estimates of trans patients are difficult to determine for a variety of reasons. Most surveys conducted for research do not currently include questions about gender identity, missing opportunities to capture even basic demographic information about transgender populations (Meerwijk and Sevelius 2017). Similarly, the United States Census and other national demographic data repositories (birth certificates, Department of Motor Vehicle records, etc.) do not include information about gender identity or discrepancies in legal sex versus sex assigned at birth (Meerwijk and Sevelius 2017). While we do not have data to effectively determine the number of trans people who live in our hospital’s catchment area, we do know that a previous study at our institution captured at least 255 gender diverse patients utilizing our institution for primary care from 2015 to 2018 (Stewart, Lee, and Damiano 2020, 51). This number is certainly an under-representation of the total trans population, but it does serve to demonstrate that a population is present and may have a need for specialized care.
Distance to care in the context of transgender health care access has several implications. One of the primary barriers to gender-affirming surgery, heightened in rural areas, is the lack of surgeons providing this type of care. A survey conducted in 2018 by Terris-Feldman and colleagues (2020) demonstrated that only 20 of 50 US states had surgeons performing genital gender-affirming surgery (vaginoplasty, metoidioplasty, and phalloplasty). This information was gathered in the same fashion that a patient would use to find a surgeon, such as utilizing national transgender patient care forums and internet searches.
Inability to access a qualified healthcare provider was described as the primary barrier for not undergoing surgery among 41% of transgender men in another survey (Sineath et al. 2016). Even among patients with a suitable provider, there are often additional barriers such as unaffordable out-of-pocket costs, challenges with insurance coverage and time away from work, exacerbated when having to travel a greater distance (Puckett et al. 2018; Terris-Feldman et al. 2020). These issues are similar for patients seeking hormone treatment or other types of care (Puckett et al. 2018; Sineath et al. 2016). For all these reasons, we felt that expanding access to transgender care at our hospital, which serves a primarily rural population, would help to ameliorate some of the impediments to care trans patients in our area were facing.
At our institution, prior to the implementation of our clinic, there was a small group of trans patients seeking care. However, there was not an emphasis on scheduling these patients with a particular provider with interest and knowledge of gender-affirming care. For example, all providers would be capable of providing hysterectomy services; however, providers delivered variable counselling on ovarian conservation for people on testosterone and largely used risks and benefits specific to a cisgender population to guide this conversation.
The specific motivation for starting this clinic stemmed from a single transgender patient who provided feedback on their experience seeking care. The last author of this paper founded the clinic after a patient reached out to Patient Relations when the gynecology clinic refused to provide the patient care in a location outside of the gynecology office. The administrative staff denied the request for care in a different location without considering whether it could and should be offered. Reasons for not wanting to seek care at a gynecology department vary between patients, but for certain individuals, this could result in “outing” them as transgender, a concern magnified for those living in small towns. Other reasons include increased dysphoria based on the clinic environment including artwork or gendered informational brochures. The patient could not simply seek care elsewhere since, in a rural environment, there are limited options for specialty care. To find a different option for care, the patient would have needed to travel a greater distance and would risk similar insensitive care in a different office. After the patient spoke with Patient Relations, care was able to be arranged in a more appropriate location for that individual. After this event, a multidisciplinary team was assembled, including community members, to discuss how to optimally offer gynecology care to transgender and gender diverse patients in our care environment.
Before the intervention, the clinic did not have a standard process for gathering sexual orientation, gender identity, and pronouns from patients. This increased the likelihood of misgendering patients during registration, rooming, visits, and subsequent encounters. For these reasons, there was motivation to identify a small group of gender-affirming providers with specialized knowledge to provide this care. Additionally, education to the entire gynecologic clinic staff was deemed necessary, as there are often patients seen outside of the specialized gender program and staffing of auxiliary team members often varies day to day.
Program Creation
Several studies have demonstrated increasing numbers of patients presenting for gender-affirming care and treatment over time (Al-Tamimi et al. 2020; Berli et al. 2017; Canner et al. 2018; O’Bryan et al. 2018). Despite the initially small number of patients being seen in our general gynecology clinic, we knew it was likely that these patients were only a fraction of the trans population living in the area served by our medical center. Thus, the dedicated Gynecology Gender Clinic program was started in 2019 at a rural, tertiary care center to serve patients closer to home, outside of a major metropolitan area, anticipating an unmet need in the region.
This clinic provides evidence-based, multidisciplinary transgender care, including gender-affirming hysterectomies and hormone management, as well as preventative health care, routine gynecologic care, and contraceptive services. The clinic works closely with other departments, including pediatric and adult endocrinology, plastic surgery, urology, and psychiatry to provide comprehensive services to patients depending on their needs. The interdisciplinary program hired a program manager to act as patient navigator and help patients interface between departments.
The program has two half-day clinic sessions per month, however trans patients are frequently scheduled into additional open spots to better accommodate the patient’s needs or the provider’s availability. The Gynecology Gender Clinic appointment slots are kept for trans patients until seven days before the clinic to ensure adequate access. This is in contrast to non-gender program appointments that are likely to fill weeks to months in advance. Advertising for the specialty clinic involved word of mouth to referring providers in the area and a new website page. Additionally, the provider is a member of World Professional Association of Transgender Health (WPATH), which lists the provider on their website.
Prior to arriving for an appointment at the Gynecology Gender Clinic, patients are administered an online questionnaire (see Appendix A) through the patient portal. If the patient has not completed the questionnaire in advance, they are given a tablet to complete the questionnaire in the waiting room or in a private exam room. This questionnaire includes questions on chosen name, pronouns, gender identity, and sexual orientation that all automatically populate the medical record. Therefore, when the patient checks in for the visit, their name and gender are already correct in the medical record. Additionally, the questionnaire collects sex assigned at birth, screens for domestic violence, and asks a sexual history. Using branching logic based on self-reported organs, the questionnaire also collects a gynecologic history including menstrual history, cervical cancer screening, and obstetrical history. These answers are reviewed by the provider during the clinic visit and confirmed with the patient to allow additional follow-up questions when needed. The questionnaire also allows patients to indicate if they would prefer to have their visit in a non-gynecology setting. If this is the case, the provider can arrange for the visit to take place in the outpatient internal medicine clinic.
Additionally, as part of the program development, the gynecology office was assessed for inclusivity. For example, the office does not have a gendered name but rather is signified by an alphanumeric indicating its geographic location in the building (floor number and alphabetical designation). All exam rooms were also labelled with rainbow flag stickers. Part of a staff meeting was designated for gender-specific training for the auxiliary staff (i.e., medical assistants, licensed nurse assistants, registration desk staff, and secretaries). Orientation for new staff now includes two 5–10-minute videos on basic gender terminology, use of chosen name and pronouns, and the importance of offering gender-affirming care. The patient schedules for all clinic types, which are viewed by the auxiliary staff throughout the day, were updated to automatically include the patient’s chosen name and gender identity.
Methods
For this study, we conducted a retrospective chart review of transgender and gender diverse individuals who sought gynecologic care and/or underwent gender-affirming gynecologic surgery (hysterectomy, with or without oophorectomy and other concurrent procedures) at a rural 396-bed academic medical center with a connected ambulatory clinic. Participants were identified using the Electronic Medical Record (EMR, Epic Systems Corporation) with the following inclusion criteria: age over 18, presenting for health care at either our outpatient gynecology clinic or our dedicated Gynecology Gender Clinic from 2017–2020. Participants were identified in the following ways: either by having their legal sex listed in the EMR as male, or by having a gender identity in the EMR of male, transgender female, transgender male, gender nonconforming, or other. Manual chart review was performed to remove non-trans patients such as cisgender males presenting for genetic or fertility counseling visits. The study protocol was approved by our Institutional Review Board, which ensured proper protections were in place to assure patient privacy and de-identification of data (Study #02001032).
Chart review was performed manually by one author to determine the nature of the visit, as well as to monitor post-operative complications for all surgeries. Data collected from January 2017 to December 2018 was allotted to the pre-implementation period, prior to the creation of the clinic. Data from January 2019 to December 2020 represents the post-implementation period after establishment of the dedicated Gynecology Gender Clinic program.
Primary outcomes include number of patients seen, number of encounters, and data regarding gender-affirming surgeries performed, including type of surgery and route of surgery. Secondary outcomes include demographic characterization of patient population utilizing our services, including gender identity and distance from the hospital.
We used descriptive statistics to assess the total number of patients served and surgical volume for gender-affirming hysterectomies in the two years before and after the creation of a dedicated program. A two-sided chi square was used for analysis of categorical variables with significance set at p < .05.
Results
Total unique patients increased from an average of 12 per year to an average of 22 per year (83% increase). Encounter volume, meaning the total number of completed visits from all patients, increased by 84%, from 44 encounters during the pre-implementation period to 81 encounters during the post-implementation period. Hysterectomy volume increased 320% (from 5 surgeries pre-implementation to 21 post-implementation; see Table 1). While two of the five pre-implementation surgeries were open/abdominal procedures, both had gynecologic or other surgical indications beyond gender affirmation to guide surgical approach, i.e., small bowel obstruction. Routes of surgery were 100% minimally invasive in the post-implementation period, with 90% being laparoscopic and 10% transvaginal. In the post-implementation group, one patient underwent concurrent partial vaginectomy and two patients underwent chest masculinization at the time of hysterectomy. 70% of post-implementation patients chose to pursue oophorectomy, while all patients in both groups underwent salpingectomy. It is our practice to use shared decision making with patients to guide decisions around oophorectomy. It should be noted that there is very limited evidence for the potential morbidity related to oophorectomy in trans populations given that extrapolating from cisgender studies is unlikely to be fully relevant (Reilly, Fruhauf, and Martin 2019). Therefore, this conversation largely focuses on the lack of population-specific data, anticipated duration of testosterone therapy, concern for lack of access to hormones in the future for political or financial reasons, fertility preservation, and theoretical risk reduction for future adnexal pathology.
Table 1. Characterization of gender-affirming care and surgery
| Variable | Pre-implementation | Post-implementation |
|---|---|---|
| (2017-2018) | (2019-2020) | |
| Number of patients | 23 | 44 |
| Number of encounters | 44 | 81 |
| Number of surgeries | 5 | 21 |
| Type of surgery | ||
| Hysterectomy | ||
| Laparoscopic | 3 | 19 |
| Transvaginal | – | 2 |
| Abdominal | 2 | – |
| Concurrent partial vaginectomy | – | 1 |
| Concurrent chest masculinization | – | 2 |
| Bilateral salpingo-oophorectomy | 5 | 15 |
| Bilateral salpingectomy | – | 6 |
| Diagnosis code for surgery (primary) | ||
| Gender affirming | 1 | 18 |
| Abnormal uterine bleeding | 2 | 2 |
| Fibroid uterus | 1 | – |
| Endometriosis | – | 1 |
| Small bowel obstruction | 1 | – |
The pre-implementation patient population had a median age of 26, with more than half of patients under age 25 (n = 14, 61%; see Table 2). The post-implementation patient population had greater age diversity, with equal patients in the 18–25 age category (n = 19) as the 26–39 category. (n = 19). The median age was 25. The majority of the pre-implementation patients (n = 17, 74%) had private health insurance, while only 4% (n = 1) were uninsured. The post-implementation population had a larger proportion of patients with Medicaid or Medicare (n = 18, 41%), though the majority had private insurance (n = 25, 57%) and only 2% (n = 1) were uninsured.
Table 2. Patient demographic characteristics
| Variable | Pre-implementation | Post-implementation |
|---|---|---|
| (n = 23) | (n = 44) | |
| Age (at first encounter) | ||
| 18–25 | 14 (61%) | 19 (43%) |
| 26–39 | 6 (26%) | 19 (43%) |
| 40–68 | 3 (13%) | 6 (14%) |
| Race/Ethnicity | ||
| White | 21 (91%) | 39 (89%) |
| Black | – | 3 (7%) |
| Hispanic / Latine | – | 6 (14%) |
| Other | 2 (9%) | 2 (5%) |
| Body Mass Index | ||
| <18–24 | 8 (35%) | 12 (27%) |
| 25–35 | 12 (52%) | 21 (48%) |
| >35 | 3 (13%) | 10 (23%) |
| Insurance | ||
| Medicaid / Medicare | 4 (17%) | 18 (41%) |
| Private / commercial | 17 (74%) | 25 (57%) |
| Charity / uninsured | 1 (4%) | 1 (2%) |
| Not listed | – | 1 (2%) |
| Employment status | ||
| Full time / part time | 10 (43%) | 20 (45%) |
| Not employed | 8 (35%) | 5 (11%) |
| Student | 5 (22%) | 8 (18%) |
| Disabled | – | 10 (23%) |
| Not listed | – | 1 (2%) |
| Legal sex | ||
| Male | 13 (57%) | 21 (48%) |
| Female | 10 (43%) | 23 (52%) |
| Gender identity | ||
| Trans male | 8 (35%) | 25 (57%) |
| Trans female | – | 1 (2%) |
| Female | – | – |
| Male | 5 (22%) | 11 (25%) |
| Gender nonconforming | 10 (43%) | 5 (11%) |
| Other | – | 2 (5%) |
| State of residence | ||
| Clinic’s state | 16 (70%) | 23 (52%) |
| Neighbor state | 5 (22%) | 18 (41%) |
| Other | 2 (9%) | 3 (7%) |
| Distance from hospital (in miles) | ||
| 0–25 | 9 (39%) | 6 (14%) |
| 26–50 | 3 (13%) | 14 (32%) |
| 51–100 | 9 (39%) | 16 (36%) |
| >100 | 2 (9%) | 8 (18%) |
Note. Column percentages may not sum to 100% due to rounding.
The most common gender identity in the pre-implementation population was “gender nonconforming” (n = 10, 43%), while “transgender male” and “male” were also present (n = 8, 35% and n = 5, 22%, respectively). In the post-implementation group, 57% (n = 25) of patients’ gender identity was “transgender male.”
In the pre-implementation group, over two thirds of patients were residents of the clinic’s state (n = 16), while 60% traveled more than 25 miles to access care, either within the state or coming from out of state (n = 14). In the post-implementation group, half of patients were residents of the clinic’s state (n = 23) and 86% of patients lived greater than 25 miles away from the clinic, either in or out of state (n = 38).
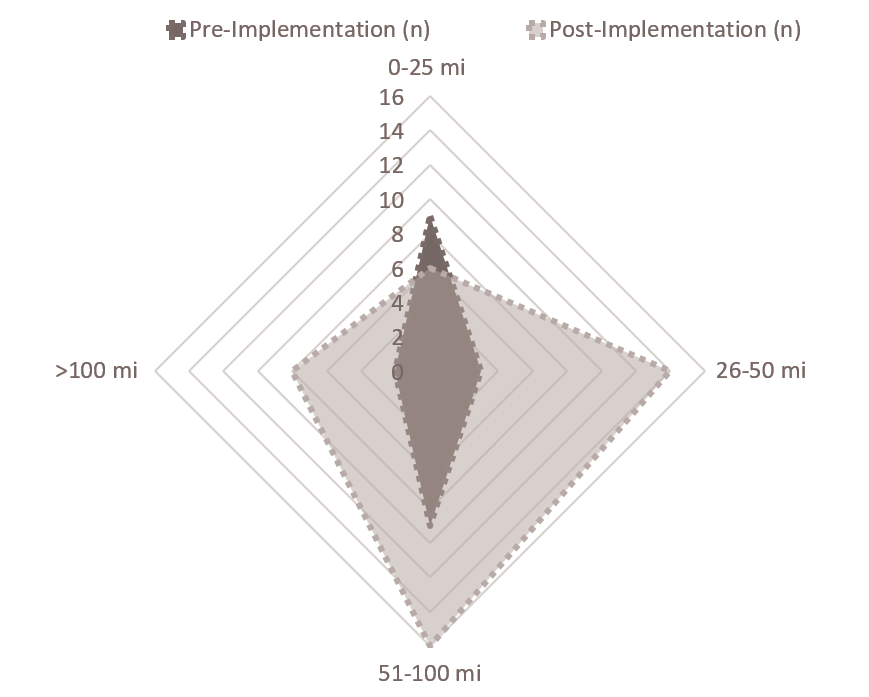
Figure 1. Patient distance (in miles) from hospital pre- and post-implementation
We also evaluated post-operative complications related to surgeries. There were no complications in the pre-implementation group (n = 5), while complications in the post-implementation period (3 complications out of 21 surgeries) included one pelvic hematoma that was managed conservatively, one case of cellulitis treated with outpatient antibiotic treatment, and an incidental diagnosis of intussusception on CT scan after presentation to the emergency department post-operatively (0% vs. 14%, p = .37). All complications were observed after laparoscopic hysterectomy.
After implementation of a dedicated clinic, gender affirmation became the primary diagnosis code for surgery (listed for 86% of surgeries), whereas this diagnosis was used for only 20% of surgeries previously. Diagnosis codes included under “gender-affirming” included gender-affirming, gender dysphoria, gender identity disorder, gender transition, transgender male, and transgender (female to male). Non-gender-affirming codes included endometriosis, abnormal uterine bleeding, and fibroid uterus.
When evaluating diagnosis codes associated with each visit, frequency of visits coded for transgender care increased by 390% when comparing the pre-implementation to post-implementation periods. Transgender care diagnosis codes included all of the ICD 10 F64.0 codes. In the post-implementation period, transgender care was the most common visit diagnosis, with 40% of visits coded as such. Preventative health care visits increased by 85%, comprising 22% of visit diagnosis codes in the post-implementation period. Routine prenatal care visits for trans-masculine patients increased 225% between the pre- and post- implementation periods and accounted for 10% of visits in the post-implementation period. Gynecology problem visits and family planning/contraception visits remained relatively stable.
Conclusions
The Gynecology Gender Clinic program was able to build a rural gynecology clinic with specific features to provide specialized care focused on each patient’s individual needs. Specifically, an electronic questionnaire was integrated with the medical record to allow patients a private mechanism to provide important information such as name, pronouns, and gender identity for those who may not feel comfortable disclosing such information to their health care provider. A dedicated program was able to provide wrap-around services for specialized gender-related healthcare, such as working in collaboration with urology or general surgery to coordinate joint surgical cases or working with behavioral health providers to obtain letters needed as a pre-requisite for insurance coverage for gender-affirming surgeries. Additionally, our clinic was able to provide continuity for patients, also addressing primary care/health maintenance needs, as well as pregnancy care.
Our results from a rural tertiary care center show that creating a dedicated clinic for transgender patients resulted in a marked increase in patient clinical and surgical volume in a two-year time period. We saw a doubling of our patient volume, as well as patient encounters. Most notable was an over 300 percent increase in surgical volume over the two-year post-implementation period. This was despite much of our post-implementation period taking place during the first months of the COVID-19 pandemic, which ceased elective surgery and decreased ambulatory clinic visits from March 2020 through June 2020. This also greatly limited surgeries for the remainder of the year, decreasing surgical volumes for all indications. These increases in clinical and surgical volume over the post-implementation period suggest that the development of a gender clinic helped meet the demand for gender- affirming services in a rural setting.
The secondary outcome was to describe the patient population utilizing these services, as gender diverse patients living in rural areas are less well characterized than those living in urban areas (O’Bryan et al. 2018; Whitehead, Shaver, and Stephenson 2016). Both the pre-implementation and post-implementation phase patients were predominantly less than 40 years old, racially homogenous (majority white, non-Hispanic/Latine), and at least half of both cohorts were residents of the clinic’s state.
In the post-implementation phase, the geographic area where our patient population lived was notably expanded, with fewer patients from within the clinic’s state, as well as increased numbers of patients coming from greater distances, with 86% of our patients driving over 25 miles to receive care, suggesting that the creation of the gender clinic expanded access to care to a wider population. The number of patients with insurance provided by Medicaid or Medicare also increased, which may represent greater socioeconomic diversity after program implementation.
Importantly, it was feasible to provide specialized gender gynecology care by dedicating physician clinical time to these patient visits. The pre-visit questionnaire was able to collect important information in advance of the visit to provide specific, patient-focused, evidence-based, care and avoid mis-gendering. This type of specialty care was not previously available in the rural setting and would have previously required travel to the nearest urban setting, approximately two hours from our center.
Strengths of our study include our position as a rural, tertiary care academic hospital. This presents a unique opportunity to explore the distinct barriers faced by the rural transgender and gender diverse population, as compared to those living in urban areas with greater availability and access to providers in all specialties and subspecialties. While our population is relatively small, it represents a unique lens that may be applicable to the greater rural transgender population. A limitation is that this study was not adequately powered to detect a difference in rare events such as post-operative complications. Our data analysis, first drawn through a data extraction from the EMR, was then corroborated with extensive manual chart review, allowing for a complete data set without missing information. Additionally, this clinic’s patient volume has continued to expand dramatically since the data for this study was analysed. One limitation is that the study design did not include pediatric patients and therefore does not represent the large volume of pediatric patients who presented for fertility preservation counseling in the post-implementation timeframe. Additionally, there may be some transfeminine patients who were inadvertently not included in analysis if both their legal sex and gender identity were listed as female.
Our study demonstrates growing demand for transgender healthcare in a rural area, both for specialized treatment and primary care utilization. To achieve equity in care for the transgender population, that is too often marginalized and medically underserved, access to both specialty as well as routine preventative care must continue to be expanded in rural areas.
References
American College of Obstetricians and Gynecologists. 2014. “Health Disparities in Rural Women.” Obstetrics and Gynecology 123 (2): 384–8. https://doi.org/10.1097/01.AOG.0000443278.06393.d6.
Al-Tamimi, Muhammed, Garry L. Pigot, Lian Elfering, Müjde Özer, Kristin de Haseth, Tim C. van de Grift, Margriet G. Mullender, Mark Bram Bouman, and Wouter B. Van der Sluis. 2020. “Genital Gender-Affirming Surgery in Transgender Men in The Netherlands from 1989 to 2018: The Evolution of Surgical Care.” Plastic and Reconstructive Surgery 145 (1): 153e–61. https://doi.org/10.1097/PRS.0000000000006385.
Berli, Jens U., Gail Knudson, Lin Fraser, Vin Tangpricha, Randi Ettner, Frederic M. Ettner, Joshua D. Safer, Julie Graham, Stan Monstrey, and Loren Schechter. 2017. “What Surgeons Need to Know about Gender Confirmation Surgery When Providing Care for Transgender Individuals: A Review.” JAMA Surgery 152 (4): 394–400. https://doi.org/10.1001/jamasurg.2016.5549.
Bradford, Judith, Sari L. Reisner, Julie A. Honnold, and Jessica Xavier. 2013. “Experiences of Transgender-Related Discrimination and Implications for Health: Results from the Virginia Transgender Health Initiative Study.” American Journal of Public Health 103 (10): 1820–29. https://doi.org/10.2105/AJPH.2012.300796.
Canner, Joseph K., Omar Harfouch, Lisa M. Kodadek, Danielle Pelaez, Devin Coon, Anaeze C. Offodile, Adil H. Haider, and Brandyn D. Lau. 2018. “Temporal Trends in Gender-Affirming Surgery among Transgender Patients in the United States.” JAMA Surgery 153 (7): 609–16. https://doi.org/10.1001/jamasurg.2017.6231.
Fantz, Corinne R. 2014. “Barriers to Quality Health Care for the Transgender Population.” Clinical Biochemistry 47 (10–11): 983–87. https://doi.org/10.1016/j.clinbiochem.2014.02.009.
Harb, Christine Y W, Lauren E Pass, Isabella C De Soriano, Adelaide Zwick, and Paul A Gilbert. 2019. “Motivators and Barriers to Accessing Sexual Health Care Services for Transgender/Genderqueer Individuals Assigned Female Sex at Birth.” Transgender Health 4 (1): 58–67. https://doi.org/10.1089/trgh.2018.0022.
Horvath, Keith J, Alex Iantaffi, Rebecca Swinburne-Romine, and Walter Bockting. 2014. “A Comparison of Mental Health, Substance Use, and Sexual Risk Behaviors Between Rural and Non-Rural Transgender Persons NIH Public Access.” Journal of Homosexuality 61 (8): 1117–30. https://doi.org/10.1080/00918369.2014.872502.
Logie, Carmen H., Candice L. Lys, Lisa Dias, Nicole Schott, Makenzie R. Zouboules, Nancy MacNeill, and Kayley Mackay. 2019. “‘Automatic Assumption of Your Gender, Sexuality and Sexual Practices Is Also Discrimination’: Exploring Sexual Healthcare Experiences and Recommendations among Sexually and Gender Diverse Persons in Arctic Canada.” Health and Social Care in the Community 27 (5): 1204–13. https://doi.org/10.1111/hsc.12757.
Meerwijk, Esther L., and Jae M. Sevelius. 2017. “Transgender Population Size in the United States: A Meta-Regression of Population-Based Probability Samples.” American Journal of Public Health 107 (2): e1–8. https://doi.org/10.2105/AJPH.2016.303578.
O’Bryan, Jane, Kimberly Leon, Carolyn Wolf-Gould, Melissa Scribani, Nancy Tallman, and Anne Gadomski. 2018. “Building a Pediatric Patient Registry to Study Health Outcomes Among Transgender and Gender Expansive Youth at a Rural Gender Clinic.” Transgender Health 3 (1): 179–89. https://doi.org/10.1089/trgh.2018.0023.
Poteat, Tonia, Danielle German, and Deanna Kerrigan. 2013. “Managing Uncertainty: A Grounded Theory of Stigma in Transgender Health Care Encounters.” Social Science and Medicine 84 (May): 22–29. https://doi.org/10.1016/j.socscimed.2013.02.019.
Puckett, Jae A., Peter Cleary, Kinton Rossman, Brian Mustanski, and Michael E. Newcomb. 2018. “Barriers to Gender-Affirming Care for Transgender and Gender Nonconforming Individuals.” Sexuality Research and Social Policy 15 (1): 48–59. https://doi.org/10.1007/s13178-017-0295-8.
Reilly, Zachary P., Timothee F. Fruhauf, and Stephen J. Martin. 2019. “Barriers to Evidence-Based Transgender Care: Knowledge Gaps in Gender-Affirming Hysterectomy and Oophorectomy.” Obstetrics and Gynecology 134 (4): 714–17. https://doi.org/10.1097/AOG.0000000000003472.
Rowan, Shon P, Christa L Lilly, Robert E Shapiro, Kacie M Kidd, Rebecca M Elmo, Robin A Altobello, and Manuel C Vallejo. 2019. “Knowledge and Attitudes of Health Care Providers Toward Transgender Patients Within a Rural Tertiary Care Center.” Transgender Health 4 (1): 24–34. https://doi.org/10.1089/trgh.2018.0050.
Sineath, R. Craig, Cory Woodyatt, Travis Sanchez, Shawn Giammattei, Theresa Gillespie, Enid Hunkeler, Ashli Owen-Smith, et al. 2016. “Determinants of and Barriers to Hormonal and Surgical Treatment Receipt Among Transgender People.” Transgender Health 1 (1): 129–36. https://doi.org/10.1089/trgh.2016.0013.
Sinnard, Morgan T, Christopher R Raines, and Stephanie L Budge. 2016. “The Association Between Geographic Location and Anxiety and Depression in Transgender Individuals: An Exploratory Study of an Online Sample.” Transgender Health 1 (1): 181–86. https://doi.org/10.1089/trgh.2016.0020.
Stewart, Talia, Y. Angie Lee, and Ella A. Damiano. 2020. “Do Transgender and Gender Diverse Individuals Receive Adequate Gynecologic Care? An Analysis of a Rural Academic Center.” Transgender Health 5 (1): 50–58. https://doi.org/10.1089/TRGH.2019.0037.
Terris-Feldman, Alexandra, Alessandra Chen, Grace Poudrier, and Maurice Garcia. 2020. “How Accessible Is Genital Gender-Affirming Surgery for Transgender Patients With Commercial and Public Health Insurance in the United States? Results of a Patient-Modeled Search for Services and a Survey of Providers.” Sexual Medicine 8 (4): 664–72. https://doi.org/10.1016/j.esxm.2020.08.005.
Tinc, Pamela J., Christopher Wolf-Gould, Carolyn Wolf-Gould, and Anne Gadomski. 2020. “Longitudinal Use of the Consolidated Framework for Implementation Research to Evaluate the Creation of a Rural Center of Excellence in Transgender Health.” International Journal of Environmental Research and Public Health 17 (23): 1–18. https://doi.org/10.3390/ijerph17239047.
Whitehead, J., John Shaver, and Rob Stephenson. 2016. “Outness, Stigma, and Primary Health Care Utilization among Rural LGBT Populations.” PLoS ONE 11 (1). https://doi.org/10.1371/journal.pone.0146139.